Much of DataDENT’s work has focused in on improving the measurement of nutrition intervention coverage. We have worked to develop new coverage indicators for Maternal, Infant, and Young Child Nutrition (MIYCN) counseling and Nutrition Sensitive Social Protection, advocated for uptake of additional coverage indicators in the Demographic and Health Survey (DHS)-8 core questionnaire and national surveys in Nigeria, India and Burkina Faso, and developed coverage measurement guidance for global actors and for the nutrition community in India.
Intervention coverage is most simply defined as the proportion of population who are eligible to receive an intervention that actually do receive it. The denominator (i.e. the number who are eligible to receive an intervention) depends on the intervention design (e.g. infant and young child feeding (IYCF) counseling should be provided to all caregivers of children 0-23 months old) and the way data are being collected (e.g. in many health sector administrative data systems the denominator is limited to those who visit facilities).
In recent years the Reproductive, Maternal, Newborn, and Child Health (RMNCH) community has expanded their understanding of coverage measurement to a full “cascade” of indicators rooted in the Tanahashi framework. As seen in Figure 1, the coverage cascade distinguishes crude intervention coverage (i.e. being reached by an intervention or program) from being reached by a delivery platform (i.e. service contact coverage), being reached by a program with a certain level of quality or adherence to standards (i.e. quality-adjusted coverage), and, ultimately, being reached with services that have the intended health impact (i.e. outcome-adjusted coverage; also called “effective coverage”).
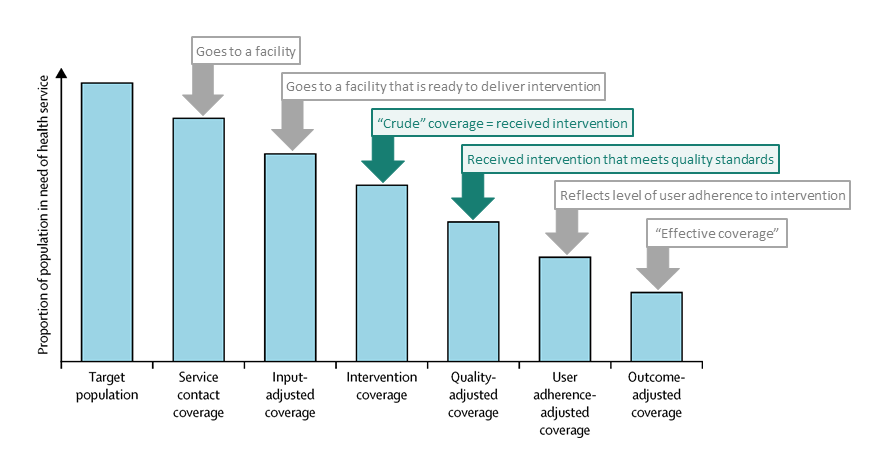
Figure 1: Unpacking the proposed standardized cascade for measuring effective coverage (Adapted from Marsh et al. (2020))
Marsh et al. (2020) illustrate how this cascade broadly applies to Growth Monitoring and Promotion (GMP) Interventions (Figure 2).
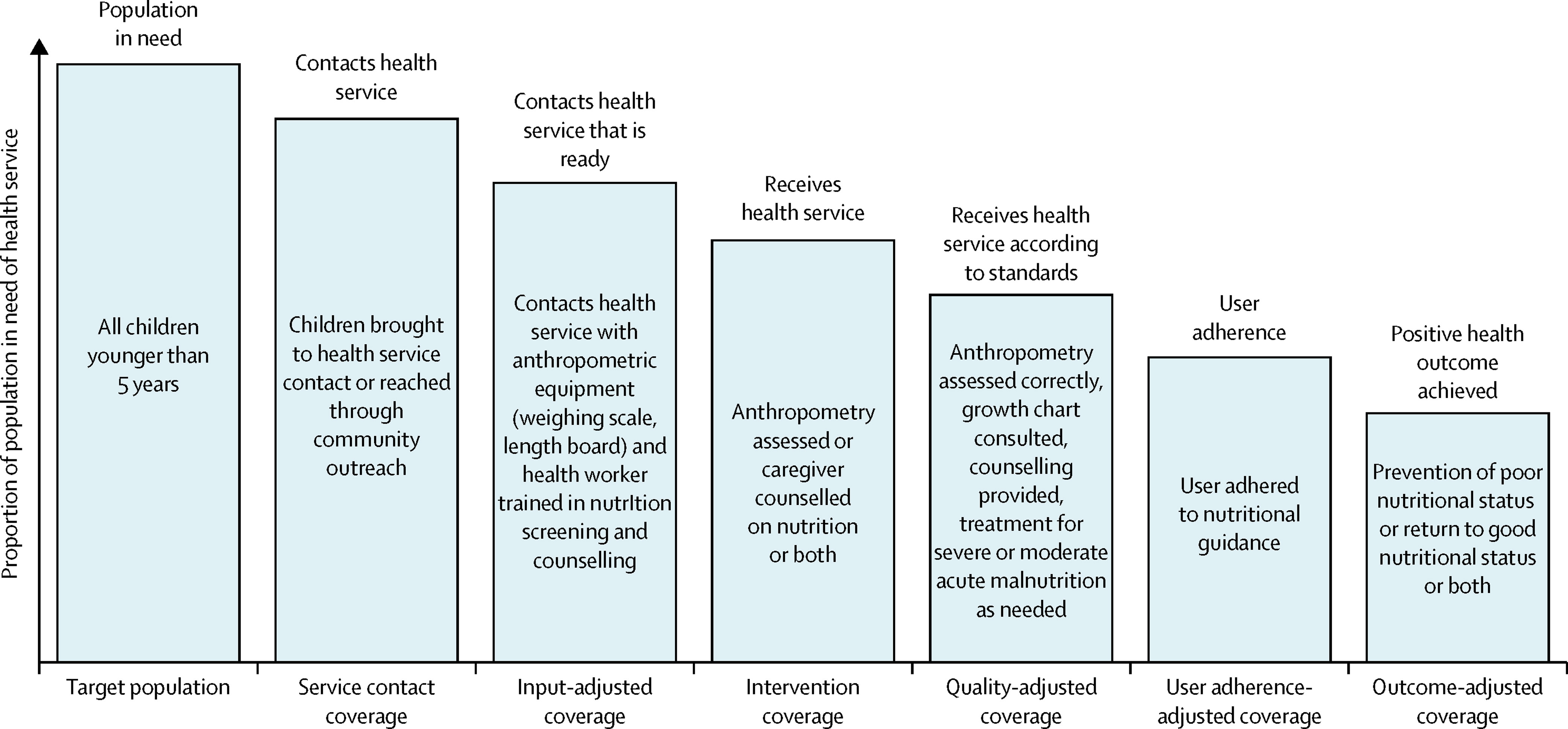
Figure 2: Health-service coverage cascade for growth monitoring, promotion, and treatment of malnutrition in children (Marsh et al. 2020)
The most common source of standardized RMNCH service readiness and quality of care data are facility-level surveys including The DHS Program’s Service Provision Assessment (SPA) survey and WHO’s Service Availability and Readiness Assessment (SARA). A number of analytical approaches have been used to link these surveys to large-scale household surveys in order to calculate quality-adjusted coverage indicators at national or subnational level. Known challenges exist in applying these methods but findings consistently show that in many contexts, quality-adjusted coverage is much lower than what crude intervention coverage indicators suggest. Figure 3 illustrates this pattern for ANC using linked data from household and facility surveys in three countries.
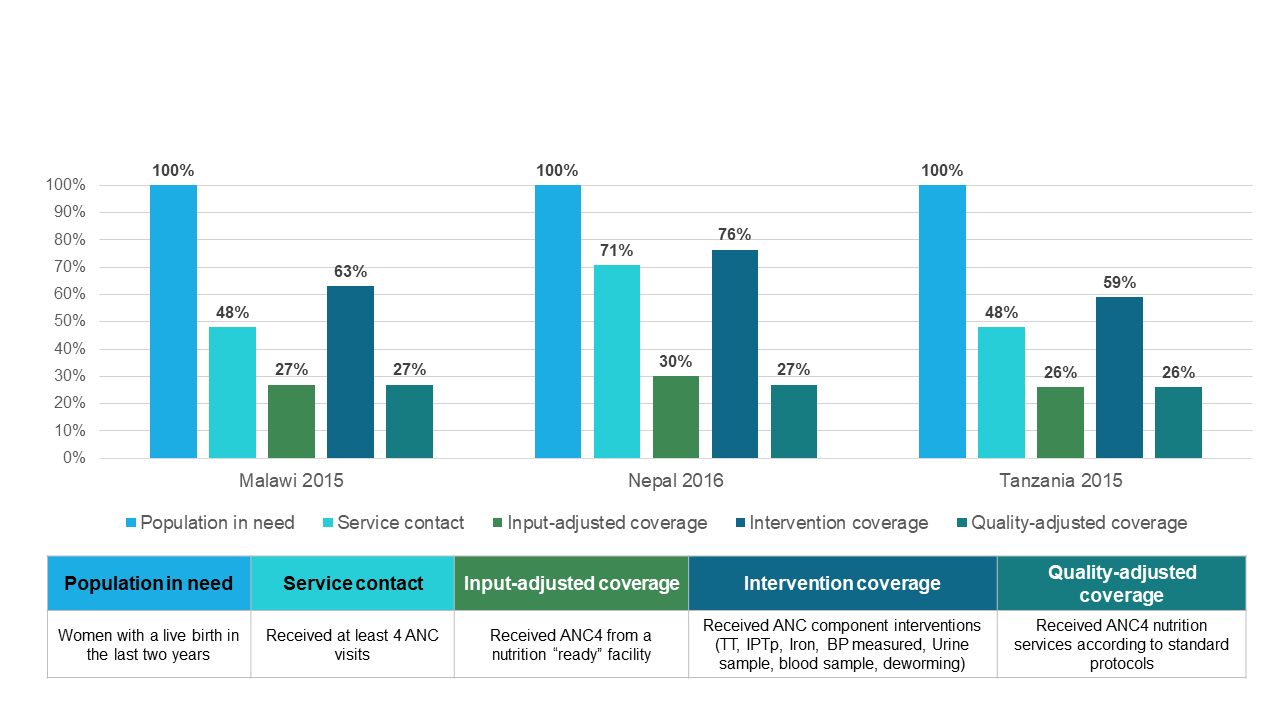
Figure 3: ANC4 Nutrition Cascade. (Figure from Ashley Sheffel, Johns Hopkins Bloomberg School of Public Health. Preliminary analysis not for citation.)
Most global and national nutrition measurement frameworks include indicators of crude intervention coverage but no indicators account for service readiness or quality of service delivery. One reason quality indicators are missing is the lack of globally-defined quality standards for many nutrition interventions. A notable exception is the Baby Friendly Hospital Initiative which has defined quality standards and associated indicators as part of 2018 Implementation Guidance. The RMNCH community has defined quality standards and associated indicators for family planning, child and maternal newborn service areas which include some nutrition-relevant standards and indicators.
Efforts by the RMNCH community to advance quality measurement continue with the WHO launching the Life Course Quality of Care Metrics Coordination Working Group which aims to develop a harmonized framework and methodology for developing, testing, and implementing quality of care indicators across the life-course. Nutrition representation in this group includes DataDENT’s lead Rebecca Heidkamp who will take part through her affiliation with WHO-UNICEF TEAM.
How is DataDENT advancing nutrition quality of care measurement?
DataDENT has carried out some targeted work to advance nutrition quality of care measurement but sees this as an area where more coordination and investment by a range of nutrition data partners is needed. From September 2020 to June 2021, DataDENT coordinated key stakeholders including UNICEF, WHO, USAID Advancing Nutrition, and MOMENTUM in providing joint recommendations for revised nutrition content in the SPA questionnaire. The SPA revision process is directed by The DHS Program and USAID, and we now await their decision on the new questionnaire (expected by early 2022). DataDENT has also collaborated with IMPROVE on carrying out an expert stakeholder survey to identify key quality of care components for nutrition interventions. Results are expected in late 2021.
